 THIS IS NOT A POLICY, PROTOCOL OR GUIDELINE. THIS IS A THOUGHT PRIMER. I AM NOT A PUBLIC HEALTH PHYSICIAN OR AN INFECTIOUS DISEASES PHYSICIAN. THESE ARE THINGS YOU SHOULD THINK ABOUT WITH YOUR TEAM WHEREVER YOU ARE IN THE WORLD. THESE ARE FOR AEROSOL GENERATING PROCEDURES. OTHER PROCEDURES, FOLLOW STANDARD LOCAL PROTOCOLS.
THIS IS NOT A POLICY, PROTOCOL OR GUIDELINE. THIS IS A THOUGHT PRIMER. I AM NOT A PUBLIC HEALTH PHYSICIAN OR AN INFECTIOUS DISEASES PHYSICIAN. THESE ARE THINGS YOU SHOULD THINK ABOUT WITH YOUR TEAM WHEREVER YOU ARE IN THE WORLD. THESE ARE FOR AEROSOL GENERATING PROCEDURES. OTHER PROCEDURES, FOLLOW STANDARD LOCAL PROTOCOLS.
You will be treating a COVID positive patient. Think about the safety of any aerosol generating procedure in this new COVID era. Modifications need to be made to mitigate the risks of spreading the virus. We need to protect the patient and healthcare staff.
What do we know?
The upper respiratory tract (the nose, nasopharynx, mouth, oropharynx, larynx, trachea and bronchi) are areas with high viral load. Evidence suggest that viral load in the nose and nasopharynx of non-symptomatic carriers are as high as those with symptoms. A patient could have no symptoms and yet carry the same amount of virus in the nose, and oral secretions. Data from China and Europe suggests that ENT surgeons have been unexpectedly hit hard with high numbers falling ill and some have died due to the virus. Studies have shown that tracheobronchial secretions carry the highest concentration of virus and followed by mucous and saliva. In some patients the virus can be detected in saliva weeks after the symptom onset. The virus has not been detected in urine or breastmilk.
What does this mean?
If you are an anaesthetist, ENT surgeon, Head & Neck surgeon, dental, maxillofacial surgeon, respiratory physician or anyone else doing procedures in the Airway mucosa, you must modify your procedures based on COVID risks. Any procedures involving the nose, oral cavity and airway pose a risk of dissemination of virus. Any general anaesthetic involving bag and masking, ventilation, intubation, supraglottic airway device, nasal surgery (rhinoplasty, septoplasty sinus surgery, adenoidectomy), oral surgery (maxillofacial, dental, tonsillectomy) and airway interventions (bronchoscopy, laryngoscopy) etc are all high risk aerosol generating procedures (AGPs).
What must we do?
1. Risk assess the patient. Can we get a COVID status on the patient? If we cannot get a COVID test pre-procedure, assess the risk based on history and examination (contact with positive COVID, travel history, etc.). Some institutions may afford you the luxury of doing 2 tests 48 hours apart to confirm the status. This is not possible in all places. Tests are not perfect so they may give a false reassurance and false negatives.
2. Risk assess the procedure and modify accordingly. Can we delay the procedure? Do we have other alternatives? Can we modify the surgical approaches? Can we use a different technique or tool to reduce the aerosolisation?
What if we have to proceed with the procedure?
Modify and mitigate the risks as a team. Communicate. Communicate. Communicate.
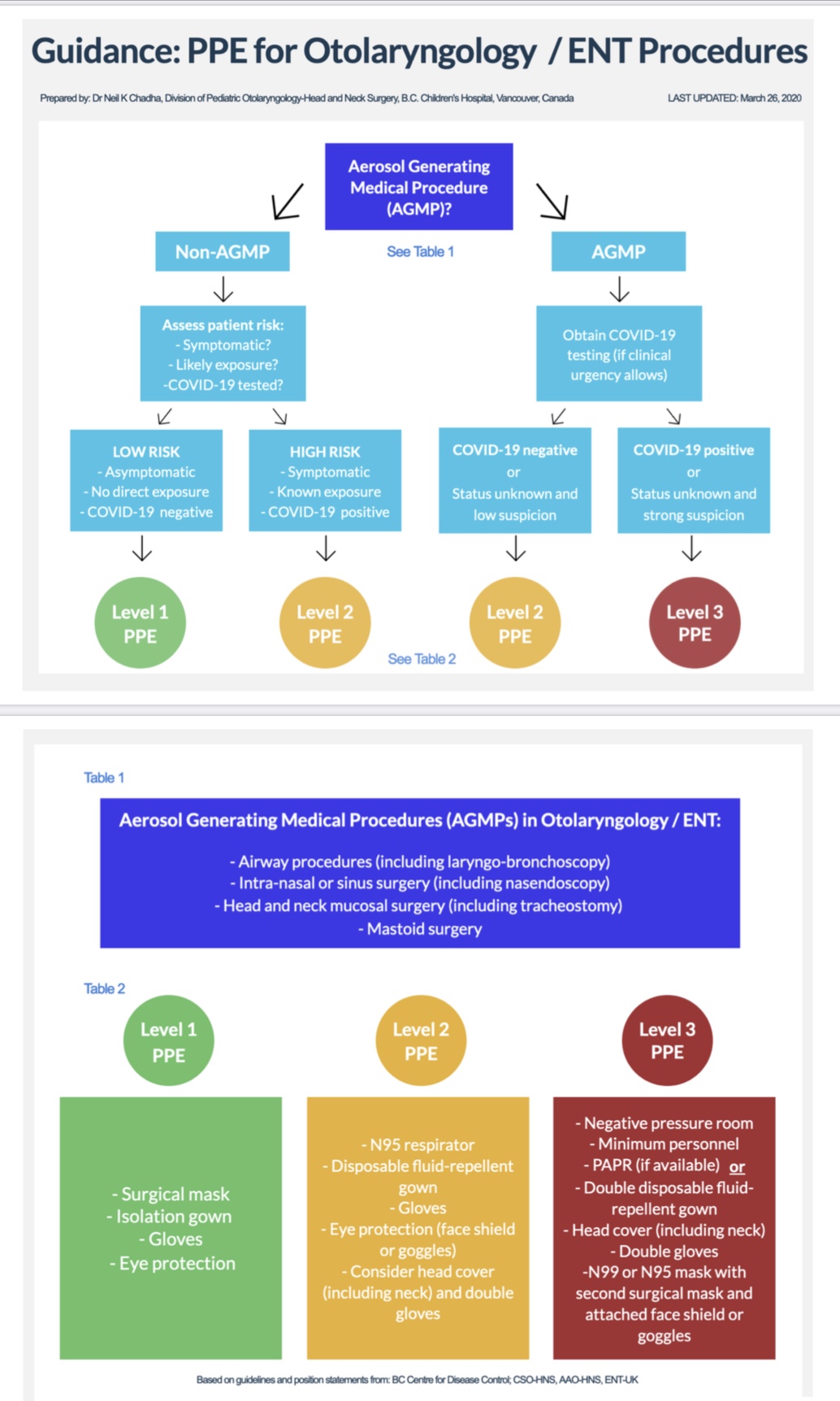
Consider 3 possible levels of risk:
These are suggestions. You need to check your local area guidelines.
GREEN: standard precaution for negative COVID patients and non aerosol generating procedure. Surgical mask, eye cover, & gloves for a non-ENT procedure. Eg. Neck dissection, thyroidectomy, etc.
YELLOW: for AGPs with negative COVID or very low suspicion of COVID. N95 mask, face shield, long sleeve gowns and gloves. Eg for mastoidectomy, FESS or tonsillectomy. Should intubation fall into this category?
RED: for COVID positive AGPs. PAPRs and the maximal PPE available at your institution. Eg. an urgent FESS in a COVID positive patient.
This diagram from the Canadian Society of Otolaryngology Head & Neck Surgery. THIS MAY NOT BE POSSIBLE IN EVERY PART OF THE WORLD.
Pre-operative considerations
Mask on the patient. Isolation. Reduce staff contact. One family member, one staff, reduce movements. Reduce exposure to other patients. Do not wait at holding bay or waiting room. Bring patient from emergency or ward direct to operating theatre.
Induction
Standard precautions. Assess level of risk Green, Yellow or Red. Reduce staff contact. Bag and mask, intubate under plastic drape. Seal the airway. Consider avoiding high flow oxygen, CPAP, Laryngeal mask etc. CHECK WITH YOUR LOCAL ANAESTHESIA TEAM.
Procedure
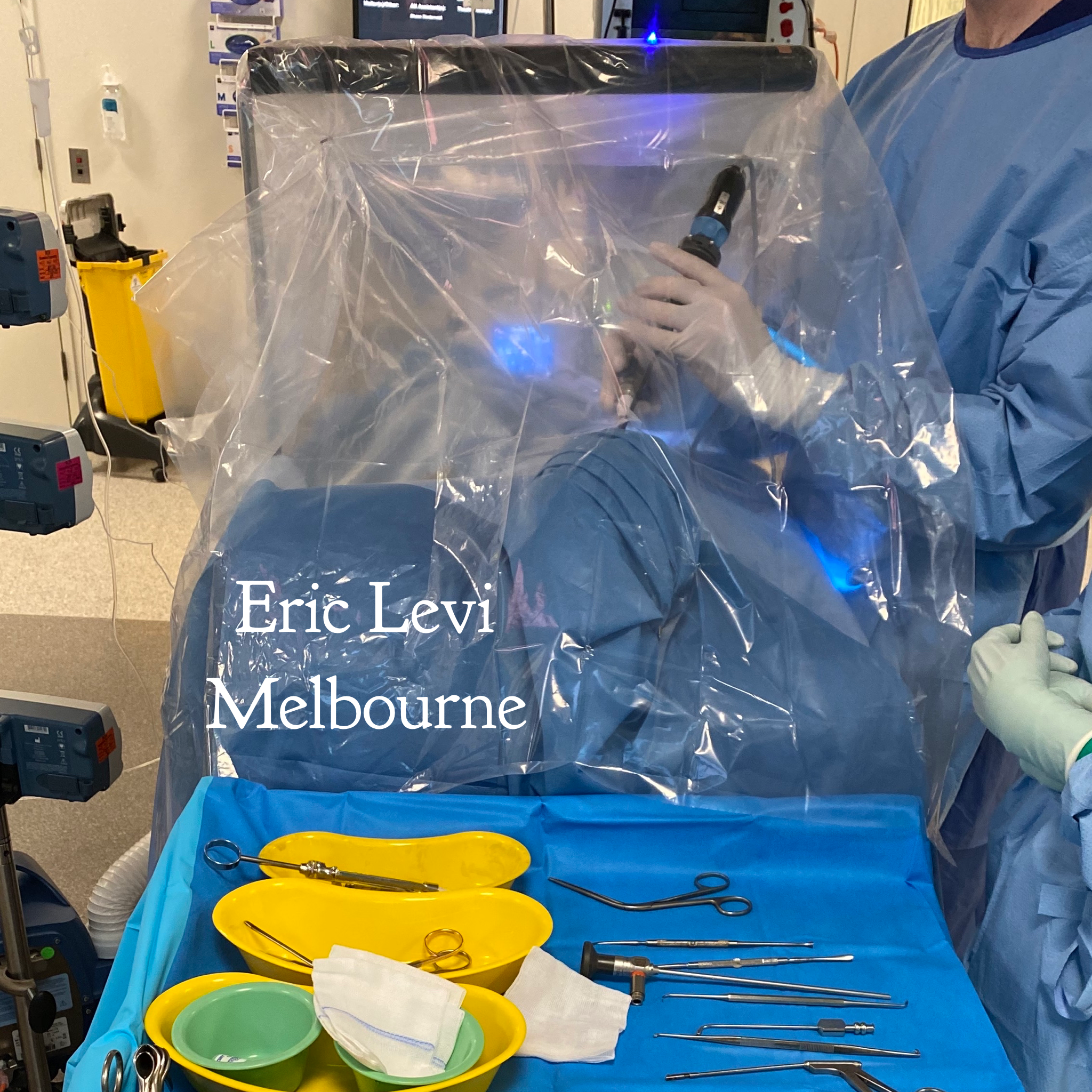
Modify techniques. Can you operate under a plastic drape? Example here. Any mucosal specimens (eg sinus debris, tonsils etc, need to be placed in a sealed container immediately). Pictures of modifications to surgical techniques below. Modify your technique accordingly so as to mitigate the risks to the staff in theatre. Reduce personnel present. Add suction device. Negative pressure theatre. Check theatre airflow. Meticulous PPE. Buddy up so someone is always catching you and checking on you. Modifications offered here. CHECK YOUR LOCAL AREA GUIDELINES.

Modification to oral surgery under a plastic drape.


Emergence & Recovery
Wake the patient in theatre. Avoid coughing in recovery. Mask on patient. Go to an isolated area in recovery. One staff member to recover. Then straight to the ward. ASSESS RISK AND DISCUSS WITH YOUR LOCAL AREA TEAMS.
Turnover
Time to allow clean up and air circulation in theatre. Wipe down everything based on levels of risk.
Closure
Communicate, Communicate, Communicate. In my experience, every single time I ask the team to do a COVID run or simulation, new gaps in knowledge and practice are identified and resolved. Morale and team work is strengthened.
Practice it. This is our new normal for the next few months.
REMEMBER TO WORK WITH YOUR LOCAL AUTHORITIES WHO ARE BALANCING INDIVIDUAL NEEDS, PUBLIC HEALTH NEEDS AND THE REALITY OF FINITE RESOURCES.

