Doctor comes from the Latin “docero”, meaning: teacher. Etymologically speaking, my primary role as a doctor is to teach. Though, to be clear, I feel that my primary role is to care. Firstly, with my actions (warm welcome, listening ear, caring focus, compassionate stance), prior to even teaching and treating with words, medications, or the scalpel.… Read more
Big Step Sunday
Seasons come and go. Life is a journey with many detours. The big story of my life has many chapters in it yet to be written. Just when I thought I had climbed one summit and sat down to rest, a voice inside tells me, “Stand up, pick up your mat and go.… Read more
How to treat a nose bleed
Nose bleeds (epistaxis) is extremely common. Not every patient requires cauterisation. About 97% of all nose bleeds occur at the front of the nose on the septum (midline) as there are major vessels that arise from the floor of the nose to supply the septum.… Read more
Decisions before birth
This talk was presented on the 13th of September at #CODA22.
Wominjeka. Welcome. We make hundreds of decisions every single day. What you wear, who you speak to, latte, piccolo, magic, soy, almond, oat milk, lactose free, or if you’re not from Melbourne, black or white coffee.… Read more
Mental health and the pandemic
Writing is my therapy. I am not a mental health clinician. I am just a surgeon who grapple with these issues within myself, my colleagues and the patients I see daily. Many of you are much more experienced and better trained to speak into this space.… Read more
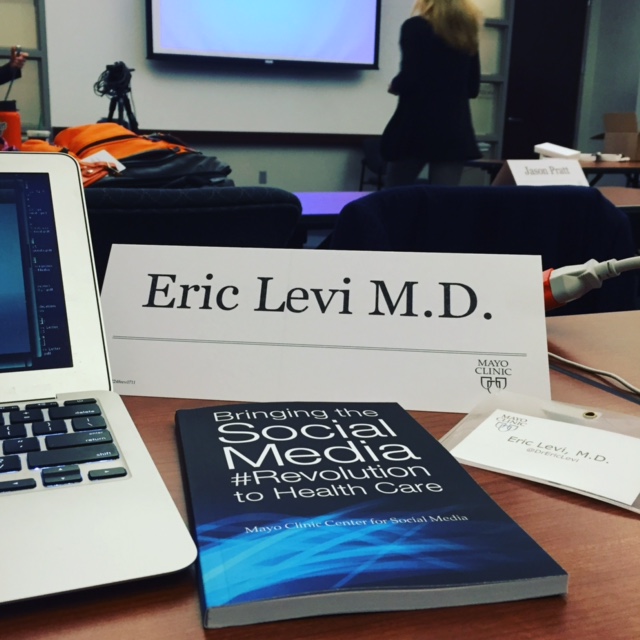
Do I need an online presence?
Do I need an online presence?
Short answer: Yes.
Long answer: It depends on the purpose.
Asking if any clinician needs to have an online presence is akin to asking in the 1970s if one needed a fax machine, in 1980s if one needed an email address or in 1990s if one needed a mobile phone.… Read more
Tips for Virtual Presentation

Thanks to COVID19, we now live in a physically-distanced virtual world. Online virtual conferences and meetings are becoming the norm. This is a great opportunity to increase our worldwide connectivity across geographical lines. Virtual meetings mean that more people can attend and less unnecessary travels are undertaken (good for the earth!).… Read more
COVID Roller Coaster

This article was published on the Australian Society of Otolaryngology Head & Neck Surgery Newsletter Summer 2020 Edition.
It was eerie. After finishing up an emergency case at 8pm, I said goodbye to the anaesthetist and the nursing staff. The usual relief of finishing a difficult case was absent.… Read more
COVID emotions
Talk presented at #NotYoga2020 Symposium Dec 2020.

I have a question for us. What do you think is our greatest asset in this pandemic?
What is the most important asset that we need to protect during this pandemic? If you’re in leadership positions, you may consider that the team or the institution as something you need to guard.… Read more
Healthcare Workers Australia: Leadership in Uncertain Times

This article is posted on Healthcare Workers Australia.
“We’re over it.” Many of us, health care workers or not, have overtly or covertly expressed this state of being. The ever-changing protocols, the hybrid telehealth clinics, the endless zoom meetings, the cancelled conferences, the restrictions, the distancing, the lack of human touch, the masked smiles.… Read more