From my ENT colleagues and for my ENT colleagues across the Tasman as of 31st March 2020. THINGS CHANGE ALL THE TIME, RAPIDLY. THIS ADVICE MAY BE INVALID IN A FEW DAYS.
Note the risk management of Aerosol-Generating Procedures and preoperative assessment.… Read more


 THIS IS NOT A POLICY, PROTOCOL OR GUIDELINE. THIS IS A THOUGHT PRIMER. I AM NOT A PUBLIC HEALTH PHYSICIAN OR AN INFECTIOUS DISEASES PHYSICIAN. THESE ARE THINGS YOU SHOULD THINK ABOUT WITH YOUR TEAM WHEREVER YOU ARE IN THE WORLD.…
THIS IS NOT A POLICY, PROTOCOL OR GUIDELINE. THIS IS A THOUGHT PRIMER. I AM NOT A PUBLIC HEALTH PHYSICIAN OR AN INFECTIOUS DISEASES PHYSICIAN. THESE ARE THINGS YOU SHOULD THINK ABOUT WITH YOUR TEAM WHEREVER YOU ARE IN THE WORLD.… 
 Brace. Brace. Brace.
Brace. Brace. Brace.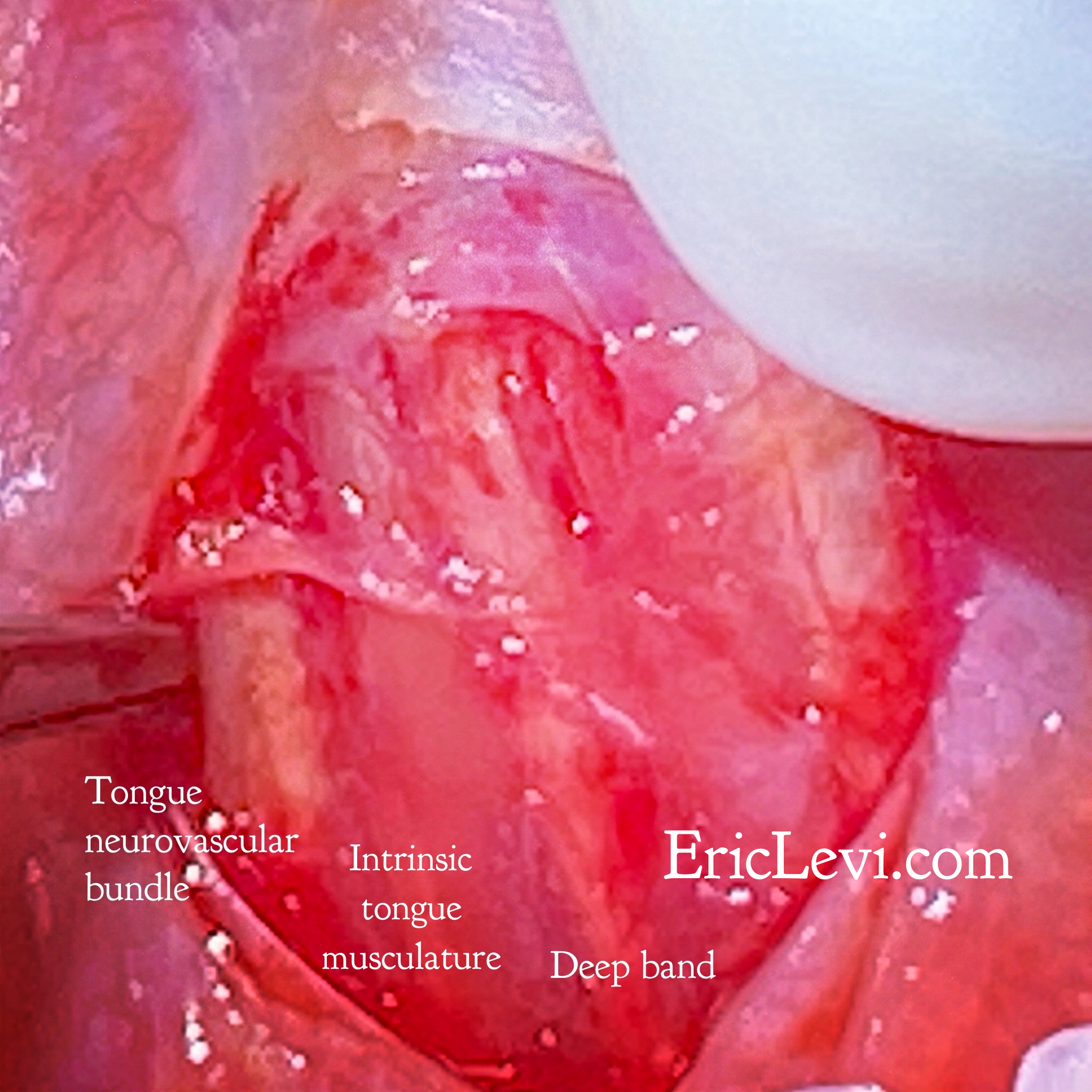 I sincerely empathise with the many mothers who are struggling with breastfeeding and who are confused about the role of tongue ties in breastfeeding, swallowing, sleep and speech. I hope I can write something of value to help you navigate this issue.…
I sincerely empathise with the many mothers who are struggling with breastfeeding and who are confused about the role of tongue ties in breastfeeding, swallowing, sleep and speech. I hope I can write something of value to help you navigate this issue.… 

 …
… 
 …
…