 I sincerely empathise with the many mothers who are struggling with breastfeeding and who are confused about the role of tongue ties in breastfeeding, swallowing, sleep and speech. I hope I can write something of value to help you navigate this issue. This is written as an opinion piece, not a scientific paper. This is an evolving subject and as more evidence is gathered, my opinion and practice patterns will change. For those clinicians (ENT surgeons, paediatricians, neonatologists, dentists, myofunctional therapist, speech pathologist, lactation consultant, etc.) scrutinising my opinion, please be mindful that in the midst of this clinical debate, we have a parent and a child who needs information and support. This is my personal opinion and not those of any organisations I am associated with. I am neither “anti” nor “pro” tongue and lip ties. I am pro better understanding of the condition. I am pro better care for the parent and child. I am pro better treatment for the child.
I sincerely empathise with the many mothers who are struggling with breastfeeding and who are confused about the role of tongue ties in breastfeeding, swallowing, sleep and speech. I hope I can write something of value to help you navigate this issue. This is written as an opinion piece, not a scientific paper. This is an evolving subject and as more evidence is gathered, my opinion and practice patterns will change. For those clinicians (ENT surgeons, paediatricians, neonatologists, dentists, myofunctional therapist, speech pathologist, lactation consultant, etc.) scrutinising my opinion, please be mindful that in the midst of this clinical debate, we have a parent and a child who needs information and support. This is my personal opinion and not those of any organisations I am associated with. I am neither “anti” nor “pro” tongue and lip ties. I am pro better understanding of the condition. I am pro better care for the parent and child. I am pro better treatment for the child.
Who Am I?
I am a Paediatric Otolaryngologist and Adult Head & Neck surgeon in Melbourne, Australia. I trained in Melbourne and went on to do 3 years of fellowships in Canada, Brisbane and Auckland. I trained in Adult Head & Neck Cancer, Facial Plastic & Reconstructive Surgery, and Paediatric Otolaryngology. My area of focus is the Airway, Sleep and Head & Neck Tumours across the lifespan. I subspecialise in assessing and treating conditions of the airway, breathing, swallowing, sleep apnoea, salivary glands, and head & neck tumours. I am part of the complex airway team, saliva control team and vascular anomalies clinic at the Royal Children’s Hospital Melbourne. I have an Academic Tertiary Hospital appointment and a private practice. I share this with you so you know my perspective. I do turbinate reduction, sinus surgery, rhinoplasty, adenotonsillectomy, airway reconstruction, head & neck tumour excision, tongue base surgery, mandibulectomy, neck dissection, salivary gland surgery, and other complex head and neck surgery as required. I see tongue and lip tie as a small part of the big picture. I am obliged to take a global perspective and treat the whole child, not just the tongue tie.
What’s the trend?
Google trend analytics shows a markedly increased number of search of the word “tongue tie”. The Australian Medicare Benefits Schedule code for tongue tie release under 2 years of age has gone from 702 patients in the one year period of 1998-1999 to 9,714 in the 2017-2018 period. This is not even accounting for procedures done in private dental clinics and wards that may not be recorded under MBS. From a literature evidence point of view, the number of yearly published articles on tongue ties have gone from 0-7 articles per year in the 70s and 80s to 27-44 articles per year in the last 5 years. Most of them are case reports, reviews and opinions. Only 8 randomised controlled trials and 10 systematic reviews have been published in the last 10 years.
There is an undeniable exponential increasing trend in tongue tie diagnosis and treatment. Is this because we are giving birth to more babies with tongue ties, or is it because of overdiagnosis and overtreatment? Or is it simply a better understanding of the condition? Just like any medical trend, we go through pendulum swings of underdiagnosis to overtreatment before finally arriving at an evidence based reasonable practice. Sadly there are, in some geographical and online communities, an overwhelming push for tongue and lip tie release procedures. Certain practitioners are strongly advocating for tongue tie release and charging a high fee for these procedures that may or may not be necessary. Performing procedures that may not be necessary is harmful for the child. On the other hand, some practitioners are declining all tongue tie referrals and therefore undertreating kids who may need the procedure. This also is harmful for the child, the mother and the breastfeeding dyad. I have seen some amazing results from tongue tie releases, but I’ve also seen some ordinary outcomes. I’ve seen many who are referred to me after having several procedures.
Where are you in the spectrum between super-believers and super-skeptics?
Please, if you are a medical, dental or allied health professional, be mindful of your own biases of overdiagnosis or underdiagnosis. There’s a lot we know and a lot we do not know yet about tongue and lip ties. Some of our strong beliefs may be founded on limited evidence.
What is a tongue tie?
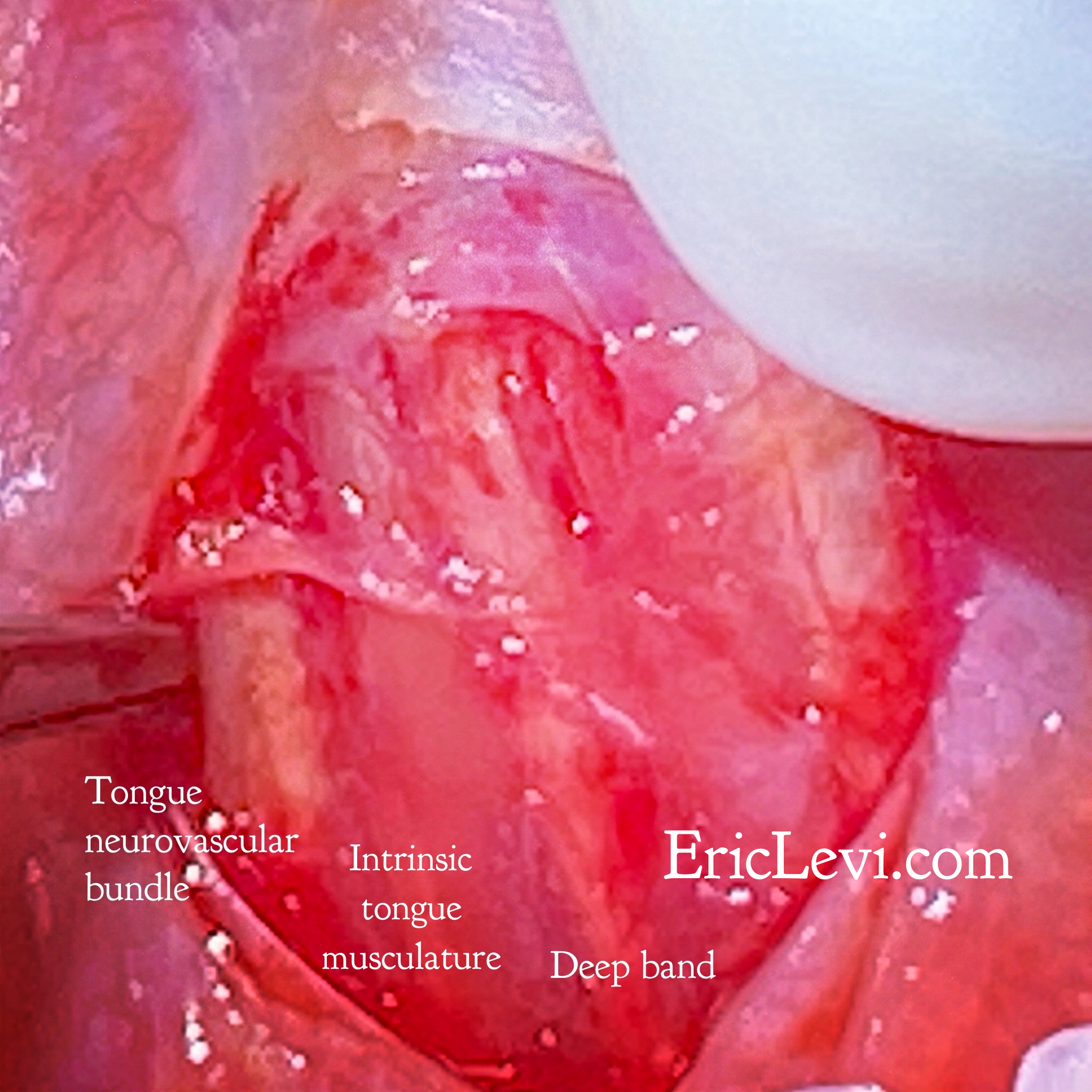
Tongue tie (or tongue frenulum or ankyloglossia) is a band of tissue (fascia) between the floor of mouth and the underside of the tongue. Dr Nikki Mills from Auckland, New Zealand has performed meticulous anatomical dissection on this anatomical region1,2 (Disclosure: Dr Mills is a friend and colleague of mine). Her study shows various different configurations of tongue ties, some superficial, others much deeper while the tongue musculature and neurovascular bundle are situated extremely close to the mucosal surface. The terms anterior and posterior tongue tie are confusing. Posterior tie does not mean it is inserting to the posterior surface of the tongue. It is a band of fascia that is situated more posteriorly than the anterior tongue tie. You may not see it but you should be able to feel it when you challenge the tongue. The grades of tongue tie (Corrylos grading) has not been completely validated, meaning, we have not studied if different grades (or class) is related to different functional limitations. It’s a description, not a measure of severity.
What is confusing about these labels and grades is that in practice we sometimes think in black and white. Does the baby have or not have a tongue tie? Is the tongue tie anterior or posterior? This black and white thinking is not helpful. We all have tongue ties to a variable degree. We all have this frenulum to a certain degree. The question is whether that tongue tie is restrictive or not. Can I use the tonsils as a comparison here? We all have tonsils. Some have bigger tonsils than others. Some big tonsils do not cause trouble. Some small tonsils cause trouble. The size of our tonsils has not been shown to accurately be related to the severity of sleep apnoea. If I removed every tonsil I see, including the asymptomatic ones, then I’m unnecessarily overservicing and harming patients. If I decline all tonsil referrals as I do not believe tonsils cause trouble, then I am also causing harm to those patients I have declined to treat. I cannot set up a Tonsil Centre to remove every tonsil referred to me, neither can I refuse all tonsil referral. The tonsil has to be assessed in the context of the whole patient. The presence of a tongue tie does not necessarily mean that it is causing harm to the child. We need to look at the impact of the tongue tie on the child as a whole. We also need to appreciate and accept that some tongue ties are problematic and need to be released.
What’s the Impact of Tongue and Lip Tie?
There is also confusion around the impact of the tongue tie on suck, swallow, sleep and speech. I would like to divide and simplify the impact into 2 general categories based on age: the infant and the older child. In the neonatal and infancy period, breastfeeding and latching is a critical function of the lip and tongue. In the older child, speech articulation and some association with sleep disordered breathing has been reported.
The baby who struggles with breastfeeding may have a tongue and/or lip tie, or they may have nasal obstruction or other possible neurological conditions. Suck – swallow-breathe reflex is an inherent reflex in an infant, so if there are limitations in the first few months, an assessment of the swallow and breathing needs to be performed by trained maternal child health nurse, lactation consultant, GP, neonatologist, paediatrician, paediatric ENT surgeon, speech pathologist or anyone else with experience. Lip tie may cause an incomplete and ineffective lip seal suction around the breast, a tongue tie may restrict the suction effect of the body of the tongue around the nipple.
In the older child, tongue tie may restrict the movement of the body of the tongue and it is thought that it positions the tongue lower down on the floor of the mouth therefore over time, resulting in a tongue that is positioned more posteriorly, a mandible that is retruded and a maxilla that takes a high arched roof position. These craniomaxillofacial changes area associated with obstructive sleep apnoea. Tongue tie in this situation may be an association, not a causation. To reverse these changes, the complete airway need to be assessed, not just the tongue tie. Releasing the tongue tie without dealing with the turbinates, septum, adenoids, tonsils or tongue base is missing the big picture.
So my child has a tongue tie. Do they need their tongue tie released?
Well, it depends on whether your child has symptoms such as difficulty latching, myofunctional disorder, obstructive sleep apnoea, or speech articulation issue. Your child needs an assessment by a GP, paediatrician, speech pathologist, dentist, lactation consultant, oromyofunctional therapist or paediatric ENT surgeon. I’ve got a tongue tie. I seem to be doing fine (ok, ok, some of you may disagree).
So my child has sleep apnoea. Do they need their tongue tie released?
Is it simple snoring, or true apnoeas? Is it allergic rhinitis causing mouth breathing or central sleep apnoea? Is it the tone of the tongue, the size of the tonsils, adenoids and turbinates? Be assessed completely by a specialist. Tongue tie may be an association and a confounder, not a cause of sleep apnoea. I have had kids referred to me for tongue tie release when their main issue is laryngomalacia or floppy larynx.
So my child has a lisp. Do they need their tongue tie released?
Is it a lisp, a stutter, an articulation error, a VPI speech or a hearing-impaired speech? Have your child assessed by a speech pathologist, audiologist, paediatrician, paediatric ENT surgeon or a specialist in the area. Sometimes, speech therapy is all you need.
So my child needs a tongue tie and upper lip tie release. What is your technique?
There is no particular technique that has been proven to be superior to others. At the end of the day, the tie has to be completely released to it’s deep attachments. These deep attachments may be between the fibres of genioglossus or intrinsic muscles of the tongue adjacent to the neurovascular bundle. There have been reported cases of significant complications when the muscle belly or vascular bundle has been cut inadvertently.
My personal technique: under General Anaesthesia and with the use of magnifying loupes I use scissors and fine bipolar diathermy at low wattage to ensure accuracy and prevent collateral thermal injury to the submandibular duct, sublingual glands and neurovascular bundle. By vision and palpation I divide the tongue tie fibres down to the muscle. I palpate for a complete give or release. I then close the mucosa over the area with dissolving sutures. Local anaesthetic is then infiltrated. Oral intake and tongue exercises are commenced immediately. They will be a little sore for 2-3 days but they can eat and drink normally, return to daily activities and commence tongue exercises immediately.
I am concerned about my child, what do I do next?
Many specialists do care. I have listed many options: Family Practitioners (GP), maternal child health nurse, lactation consultant, oromyofunctional therapist, speech therapist, paediatrician, dentist, ENT Surgeons, etc. There is good evidence that in the right patient for the right reason, tongue and upper lip tie release is effective in treating breastfeeding difficulty, speech and swallowing difficulties, and even sleep disordered breathing. We have to be careful though as this does not necessarily apply to every patient. As parents you have the best interest of your child at heart. Sometimes you need to see 2 or 3 specialists before arriving at the right advice that you are comfortable with. At the end of the day, you need to decide what is best for your child.
Concluding remarks
I hope I have given you some things to consider. This is not a perfect article. I do not have the perfect opinion. Many will disagree and that is fine. Ultimately my job as a paediatric ENT surgeon is to provide safe care, information and education. We need to do a lot more research in this arena. In the mean time I have a duty of care to provide the safest care to the child and parent in front of me based on my training and expertise in Paediatric Airway, Sleep and Head & Neck Surgery.
References
- https://onlinelibrary.wiley.com/doi/full/10.1002/ca.23343
- https://onlinelibrary.wiley.com/doi/10.1002/ca.23410

